Introduction
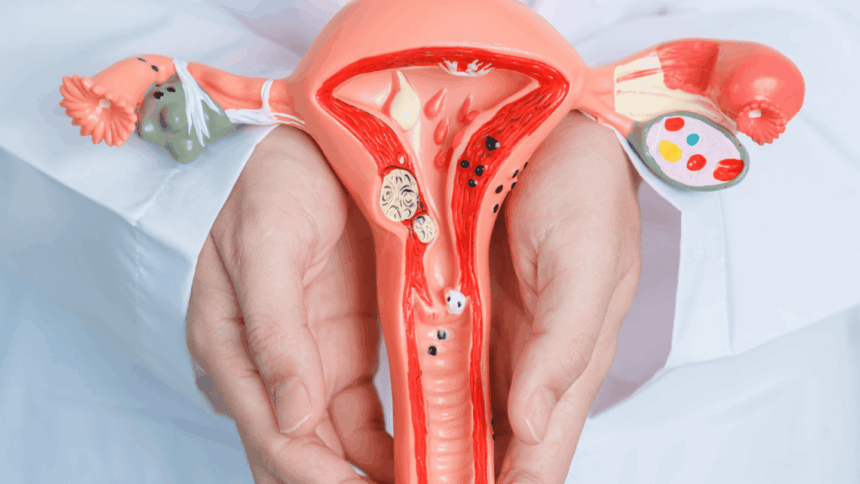
Cervical cancer remains one of the most preventable yet serious cancers affecting women worldwide. It develops in the cells of the cervix—the lower part of the uterus that connects to the vagina. While the disease can be life-threatening if left untreated, the good news is that early detection and preventive measures significantly reduce the risk. With advancements in screening methods, vaccination, and awareness campaigns, cervical cancer rates have been declining in many countries.
Understanding Cervical Cancer
Cervical cancer usually begins with precancerous changes in the cells lining the cervix. The human papillomavirus (HPV)—a common sexually transmitted infection—is the leading cause of cervical cancer. Not all HPV infections lead to cancer, but persistent infection with high-risk HPV types can cause abnormal cell growth.
Key Risk Factors
- HPV infection (especially types 16 and 18)
- Smoking
- Weak immune system
- Multiple sexual partners or early sexual activity
- Long-term use of oral contraceptives
- Family history of cervical cancer
Prevention of Cervical Cancer
1. HPV Vaccination
The HPV vaccine is one of the most effective preventive tools. It protects against the high-risk HPV strains responsible for most cervical cancers. The vaccine is recommended for both girls and boys, ideally before becoming sexually active.
2. Practicing Safe Sex
Using condoms and limiting the number of sexual partners can reduce the risk of HPV transmission.
3. Healthy Lifestyle Choices
A strong immune system helps fight infections. Quitting smoking, maintaining a balanced diet, and regular exercise can lower the risk of cervical cancer.
Screening for Cervical Cancer
1. Pap Smear Test (Pap Test)
The Pap test checks for abnormal cells in the cervix before they turn cancerous. Women aged 21 to 65 are advised to have regular Pap tests every 3 years.
2. HPV Test
This test detects the presence of high-risk HPV strains in cervical cells. It may be done alone or in combination with a Pap test (co-testing).
3. Visual Inspection with Acetic Acid (VIA)
In some regions with limited access to advanced testing, VIA is used as a cost-effective screening method.
Importance of Early Detection
Early detection through screening can identify precancerous changes before they develop into cervical cancer. When found early, cervical cancer is highly treatable with excellent survival rates. Late-stage detection, however, requires more aggressive treatments like chemotherapy and radiation, with reduced success rates.
Symptoms to Watch For
While cervical cancer may not show symptoms in its early stages, advanced stages can present with:
- Abnormal vaginal bleeding (between periods, after sex, or after menopause)
- Unusual vaginal discharge with foul odor
- Pelvic pain or pain during intercourse
Conclusion
Cervical cancer is a disease that can largely be prevented through vaccination, healthy lifestyle choices, and regular screening tests. Every woman should prioritize routine Pap or HPV tests as part of her healthcare. Early detection saves lives, and awareness is the first step toward reducing the global burden of this preventable cancer.
FAQs
Q1. At what age should women start cervical cancer screening?
Women should begin Pap smear screening at age 21, even if they are not sexually active.
Q2. Is HPV vaccination only for young girls?
No. While it is most effective before sexual activity begins, boys and men up to age 26 (and in some cases up to 45) can also benefit from HPV vaccination.
Q3. How often should Pap smears be done?
For women aged 21–29, every 3 years. For women aged 30–65, Pap plus HPV testing every 5 years, or Pap test alone every 3 years.
Q4. Can cervical cancer be inherited?
While genetics may play a role, most cases are linked to HPV infection, not hereditary factors.
Q5. What is the survival rate of cervical cancer if detected early?
When detected in the early stages, the 5-year survival rate is above 90%, making early screening crucial.